What is a Pap Smear (or a Papanicolauo’s Test)?
 Pap smears, also called cervical smears are very important for women who start having sex in their early teens. This may be because the young cervix is more vulnerable to cancerous changes when exposed to semen early in a woman’s fertile lifetime. Precancerous or cancerous changes are even more likely to occur if you have several sexual partners. The virus that promotes cervical cancers is the HPV virus – the same virus that causes genital warts.
Pap smears, also called cervical smears are very important for women who start having sex in their early teens. This may be because the young cervix is more vulnerable to cancerous changes when exposed to semen early in a woman’s fertile lifetime. Precancerous or cancerous changes are even more likely to occur if you have several sexual partners. The virus that promotes cervical cancers is the HPV virus – the same virus that causes genital warts.
Having a Pap Smear Taken
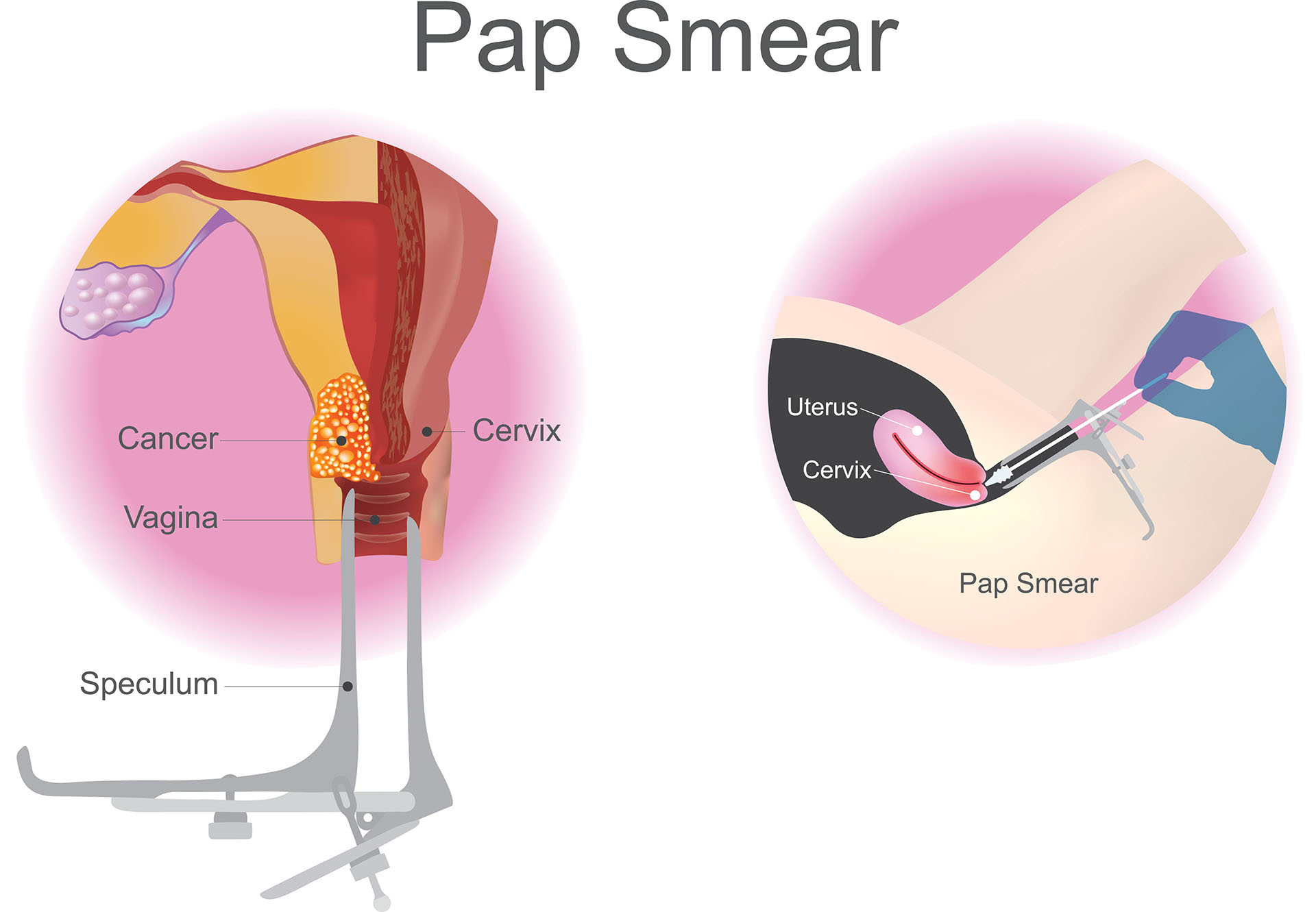
A warmed speculum (speck-you-lumm) is passed into the vagina to separate the walls so the health care provider can see your cervix (the part of the uterus that is at the very top of your vagina and is the bottom of the uterus). Cervix actually means the neck of the uterus.
![]() A wooden spatula (thinner than a tongue depressor) is wiped across the cervix, and the smear is transferred to a glass slide. Also a very long wand, much like a mascara wand is used to gently scrape the inside of the cervix. This doesn’t hurt; some women say they feel a little twinge, but it only lasts a second. This wand is also smeared on the slide and sprayed with a solution to “fix” it to the slide. The slide is then sent to a laboratory to be examined by a medical person who specializes in “reading” pap smears. The results should be available in a few days.
A wooden spatula (thinner than a tongue depressor) is wiped across the cervix, and the smear is transferred to a glass slide. Also a very long wand, much like a mascara wand is used to gently scrape the inside of the cervix. This doesn’t hurt; some women say they feel a little twinge, but it only lasts a second. This wand is also smeared on the slide and sprayed with a solution to “fix” it to the slide. The slide is then sent to a laboratory to be examined by a medical person who specializes in “reading” pap smears. The results should be available in a few days.
Note to the ladies:
If you are menstruating you should reschedule your pap smear as the blood cells make the smear difficult to “read” accurately. The same is true if there is semen on your cervix — if you had sex without a condom within 24 hours of the pap smear.
What The Results Mean
The results of a pap smear test are classified into five categories:
- Negative – Means everything was normal.
- Mild dysplasia – This means you have some abnormality and should be screened again in six months. This does NOT mean you have cancer.
- Moderate dysplasia – This means a change in the cells that requires further investigation.
- Severe dysplasia – This means there is a change in the cells that requires further investigation with another procedure.
- Abnormal cells (Class V) – These cells are cancerous.
Smear test results and action taken:
|
Result |
Action Taken |
| Negative (Normal) | None. Repeat in one year. |
| Mild Dysplasia | Repeat Pap smear in 6 months. |
| Moderate Dysplasia | Colposcopy |
| Severe Dysplasia | Colposcopy with or without cone biopsy. |
| Class V – Cancer cells | Several types of surgical techniques are used depending upon severity. |
Cervical cancer is the most easily detected and, if caught early, the most easily cured of all the cancers of the female reproductive system.
What Is a Colposcopy?
 A colposcope, a kind of large microscope, is placed at the entrance of your vagina to give a magnified view of the area of your cervix where the cells were taken from that were not normal. During a colposcopy the cells of the cervix may be stained with a solution so it will be easier to tell which ones are not normal. Some cells may be removed for more lab tests.
A colposcope, a kind of large microscope, is placed at the entrance of your vagina to give a magnified view of the area of your cervix where the cells were taken from that were not normal. During a colposcopy the cells of the cervix may be stained with a solution so it will be easier to tell which ones are not normal. Some cells may be removed for more lab tests.
A cone biopsy is where the entire layer of cells that are abnormal on the pap smear is removed by a scalpel or by a laser beam. You are not awake during this procedure. If cancerous cells are discovered, treatment is given for cervical cancer.
There is some debate now among the medical community as to how often should women have Pap smears. Some doctors say every year for the first three years after you become sexually active, others says after 3 years of negative (normal) results, every two years is fine. We believe it is wise to have a pap smear every year, but discuss this with your health care provider.
Pap Smears and Cervical Cancer: What Every Woman Should Know
by Craig L. Bissinger, MD – (Updated 8/20/2002)
How much do you know about the prevention of cervical cancer? Did you know, for example, that although it was once the number one killer of American women, it is now considered preventable by using a simple test? Of the 16,000 newly diagnosed cases and 4,800 women who will die of cervical cancer this year, almost all of them could have been prevented with a pap smear.
As a physician, I find it extremely gratifying to see women taking care of their health. It’s hard to believe that there are still millions of women who fail to keep up with annual check-ups. Prevention of disease, with an annual pap smear, is the most effective medicine possible against cervical cancer. To understand why a pap smear is the first line of defense against cervical cancer, it is important to know a few basic points about the test itself.
What Is a Pap Smear?
A pap smear is a test in which a ‘smear’ of bodily secretions, especially from the cervix, is taken from the body, and examined to detect any abnormal cells.
The cervix is composed of two types of cells. The majority of the cells are flat cells called squamous cells. They encircle the entire cervix with the exception of an area in the center, which is composed of mucus-secreting cells known as columnar cells. The two types of cells come together at an area known as the squamo-columnar junction. I retrieve a sample from this spot because the cells are actively growing and any changes in the cells can be found in here.
The Procedure
When I do a pap smear, I use an instrument called a speculum to inspect the vagina. The instrument resembles a duck’s beak with two portions that can be drawn apart to view the vagina and cervix. After carefully inserting the speculum into the vagina, I open and position it so that I can see the cervix (the tip of the uterus). With both a small wooden spatula and a brush, I scrape the surface of the cervix to obtain a sample of skin. It is a quick and relatively painless process. Women often describe the feeling as an ‘internal pinch’ when the brush touches the cervix. After I’ve obtained the sample, I rub the cells onto a glass slide and then I ‘fix’ the sample to the slide with a spray.
Human Papilloma Virus
The two cell types, squamous and columnar cells, are constantly reproducing and creating new cells. This process of cell division progresses normally until something triggers a change. In almost all cases, the changes are caused by a virus known as human papilloma virus (HPV), also known as genital warts. The virus is introduced through sexual intercourse and has the unique ability to infect the dividing cells of the cervix. Once inside the cell, HPV inserts itself into the DNA of the cervical cells and alters their ability to produce new cells. A simple way to understand the role of HPV is to imagine the virus as a foreman on a production line. The foreman has given new instructions to the workers to alter the way a part is made. In the case of HPV, defective cells are’ the new parts’, and they will in turn produce more and more defective cells. Over the course of many years, the cells tend to become cancerous. This process takes a long time, and an annual pap smear can detect some of these changes early on.
What Happens in the Lab?
The specimen is sent to a laboratory where it is treated with special stains to highlight the cells for study. A specially trained technician will examine the slide to determine if it is normal. The results are then given to the physician who performed the pap smear. In order to maintain a high level of quality, 10% of all the slides are reviewed at the laboratory. In addition, many labs have physicians known as pathologists who review a select sample of the slides, especially the abnormal ones, to ensure the accuracy of the tests.
Pap Smear Accuracy
Even in the best labs, the pap smear is only 80% accurate. This means that some abnormalities will not be detected or a test may be interpreted as having a problem where none exists. This can lead to a great deal of confusion and anxiety for the patient. Fortunately, the cell changes responsible for cervical cancer take many years to develop and with repeated pap smears, the chance of missing an abnormality is very remote. Still, the idea that an abnormality might be undetected causes much concern among my patients. I use a little math to ease their fears. Each year you have a 20% (which is 0.2) chance of a falsely normal pap smear. If we did a pap yearly for three years, your risk of missing an abnormality would be 0.2 x 0.2 x 0.2, which equals 0.008 or 0.8%. This is less than one percent! This is a comforting percentage for my patients, and another reason why annual pap smears are so important.
The Lab Results
After your pap smear is examined at the lab, your physician will receive a report describing the results of your pap smear as either satisfactory or unsatisfactory. On the report, there will be comments about the type of cells seen: A recommendation of follow-up care will be accompany the results. Listed below are the possible diagnoses:
Normal: The cells appear normal and a follow-up pap should be done the following year.
Unsatisfactory pap smear: I tell my patients that an unsatisfactory pap smear is a “do over”. It means that there was a problem with the preparation or staining of the slide, or there was an interpretation error, or there were not enough cells retrieved for proper evaluation.
Inflammation: This means that there are no changes in the cervical cells that would indicate cancer, but there are inflammatory changes in the cells environment.
Benign changes: These are changes within the cervical cells themselves that have not yet progressed to be cancerous. This should be followed regularly, I would recommend a re-check in one year.
Atypical squamous (glandular) cells of undetermined significance (ASCUS or ASGUS): This diagnosis is the most confusing to patients. Basically it means that the person at the lab who evaluated the slide felt that some of the cells were slightly abnormal but not abnormal enough to warrant more aggressive evaluation. This may occur in situations associated with mild infections in the vagina or during the postpartum (after delivery of a baby) or menopausal time periods. * Pap smears should be repeated 3 to 6 months after this diagnosis. If the follow-up smear is normal, you should resume yearly pap smear testing. If the repeat test is still ‘ASCUS’, you should have a colposcopy (described below)…
Low-grade squamous intraepithelial lesion (LGSIL): This result requires further testing by means of a colposcopy. A low-grade squamous intraepithelial lesion represents the mildest cervical change, though 15% of these abnormalities will progress toward cancer (Don’t worry. It will take more than 5 years to get there). Many physicians recommend treating these lesions by destroying the abnormal cells. 60% of these lesions will disappear on their own without treatment, and there are some doctors who prefer to follow patients in this group with repeated pap smears and colposcopy instead of treatment.
You may wonder why many physicians treat these patients if most of them will heal on their own. A doctor’s internal monologue goes something like this: “Forty percent need therapy, but which ones? Should I wait and find out? What happens if my patient fails to follow-up or moves away?” Without answers to these questions, many doctors prefer to offer treatment when a patient is diagnosed with a low-grade squamous intraepithelial lesion.
High-grade squamous intraepithelial lesion (HGSIL): This result also requires further testing by colposcopy and represents a pre-malignant condition, which must be treated aggressively by destroying the abnormal cells. There is no question about this diagnosis. Failure to treat will lead to cancer in many patients.
Cervical Cancer: This is a rare diagnosis, and the patient should be referred to a gynecological oncologist for management and treatment.
Other Types of Cervical Testing
In some cases, I recommend an additional test called a colposcopy (pronounced coal-pa-scoe-pee).
Colposcopy
In a colposcopy, as with a pap smear, your doctor will use a speculum to see the cervix. The cervix is cleaned with a vinegar solution. Using a special set of ‘binoculars’ mounted on a stand (colposcope), the doctor shines light on the cervix and takes a biopsy (sample of cells for study) of all areas that look suspicious. In addition, some of the cells on the uterine wall will be gently scraped off and sent to the lab. This is done to check for any abnormal cells that may not be obvious.
At the time of the colposcopy, I can usually predict the diagnosis based on the appearance of the cervix, which is a tremendous relief to the patient. When the biopsy results return from the lab, I compare those results with my own findings at the time of the actual colposcopy procedure. The biopsy results and procedural findings should be consistent. If they are not, I perform additional tests.
LEEP
A loop electrical excision procedure of the transformation zone, referred to as LEEP, is another diagnostic procedure that has become very popular. It involves using a live, electric wire loop to scoop out a small piece of tissue from the squamo-columnar junction. A sample of the cells on the uterine wall is also scraped during this procedure. Both samples are then sent to a lab for analysis. This test requires local anesthesia, given as an injection similar to a shot of novocaine at the dentist, but takes only seconds to perform. You should expect to have a watery discharge for up to 2 weeks following this procedure, which is normal.
Cone Biopsy
In any cervical/uterine test, the physician must be able to see the entire cervical opening to make a proper evaluation. In certain circumstances this is not possible and further testing is needed. In the case that a physician cannot see or evaluate the cervix properly, a cone biopsy is recommended.
This procedure typically involves a trip to the operating room and many physicians will request that you have some sedation or general anesthesia when doing this type of procedure. There are some doctors, however, who will use a local anesthesia for a cone biopsy. The procedure involves cutting out a central portion of the cervix (which includes the squamo-columnar junction) and sending it to the lab. This can be done with a knife, a laser, or with the LEEP method. The tissue sample actually looks like an ice cream cone, hence the name. Because it involves cutting out a larger piece of tissue, cone biopsy is considered more likely to find any abnormal tissue. The surgery takes 20 to 40 minutes to complete. Post-operatively, there is little pain. Most of my patients who have had a cone performed say it feels like menstrual pain and is easily relieved with Ibuprofen.
A cone biopsy should be performed if:
- The diagnosis is unclear from a previous colposcopy biopsy.
- The entire cervix cannot be visualized by colposcopy.
- Abnormal cells are found along the uterine wall.
- There is suspicion of cervical cancer.
Treatment
The basic job of any cervical treatment is to destroy abnormal cells. Once abnormal cells are destroyed, the cervix has a chance to regenerate healthy cells. Biopsy results usually take between 2 and 7 days to come back. Before diagnosis, I like to outline for my patients how I will manage their treatment in the case that they need treatment. I explain to my patients that any of the available cervical treatments will cure between 90% and 95% of patients.
Cryosurgery
Cryosurgery has been a “treatment work horse” for many years. It involves a process of freezing the cervix and destroying the entire junction between the squamous and columnar cells. It is a quick, office-based procedure and causes minimal discomfort. In general, a few Advil or Tylenol in advance of the procedure will suffice as pain medication. After the procedure, patients will experience watery discharge for up to 2 weeks.
Laser Surgery
Laser treatment was an appealing option in the past and still has a role in certain circumstances if your doctor is comfortable using it. Treatment using a laser involves the use of high energy to vaporize an abnormal area. It takes longer than cryosurgery and is more uncomfortable. Sometimes local anesthesia is used to make the procedure more comfortable. Patients will experience watery discharge for up to 2 weeks.
Electrocautery
Electrocautery uses electrical energy to burn away abnormal cervical tissue. It is a quick procedure, which typically requires local anesthesia to perform. As with all these procedures, a watery discharge should be expected for up to 2 weeks.
Cone Biopsy
The cone biopsy was described above, but it is both a diagnostic and a therapeutic treatment. If the cone biopsy is found to have removed all abnormal cells when examined in the lab (has clean margins) it will have successfully treated as well as diagnosed the problem. In many patients, it is just as effective as hysterectomy for pre-cancers of the cervix.
Follow-Up
Following treatment, I suggest that patients have pap smears every 3 months for a full year to make sure that any recurrence of abnormal cells are promptly found. In the second year after treatment, I extend the interval between tests to 6 months. Thereafter, yearly pap smears are recommended. In the event that a recurrent abnormal pap smearis obtained, you should start from scratch and again go through the process of colposcopy, biopsy, and treatment.
Conclusion
The pap smear is an excellent screening test to help prevent and detect cervical cancer. With these routine tests, you can help make cervical cancer a thing of the past. The time you have taken here to learn about this important health topic is well spent. It is up to each of us to take charge of our own health. Don’t be afraid to ask your doctor questions. Be assertive. Nobody is as interested in your health as you!
Good luck and good health to you.
Craig L. Bissinger, MD
© 2002 Healthology, Inc.
To our Cervical Cancer article…
For more on Genital Warts and HPV and the Gardacil® Vaccine.
For more up-to-date information, check out these resources.
You can find out more about Pap tests by contacting the
National Women’s Health Information Center (NWHIC) at
1-800-994-9662 or the following organizations:
Cancer Information Service, NCI, NIH, HHS
Phone Number: (800) 422-6237
Internet Address: http://cis.nci.nih.gov
American College of Obstetricians and Gynecologists (ACOG) Resource Center
Phone Number: (800) 762-2264 x 192 (for publications requests only)
Internet Address: http://www.acog.org
American Cancer Society
Phone Number: 1-800-227-2345
Internet Address: http://www.cancer.org
National Cervical Cancer Coalition (NCCC)
Phone Number: (800) 685-5531
Internet Address: http://www.nccc-online.org
Planned Parenthood Federation of America
Phone Number: (800) 230-7526
Centers for Disease Control
National Breast and Cervical Cancer Early Detection Program
Phone Number: (888) 842-6355
Internet Address: http://www.cdc.gov/cancer/nbccedp