What Are Genital Warts?
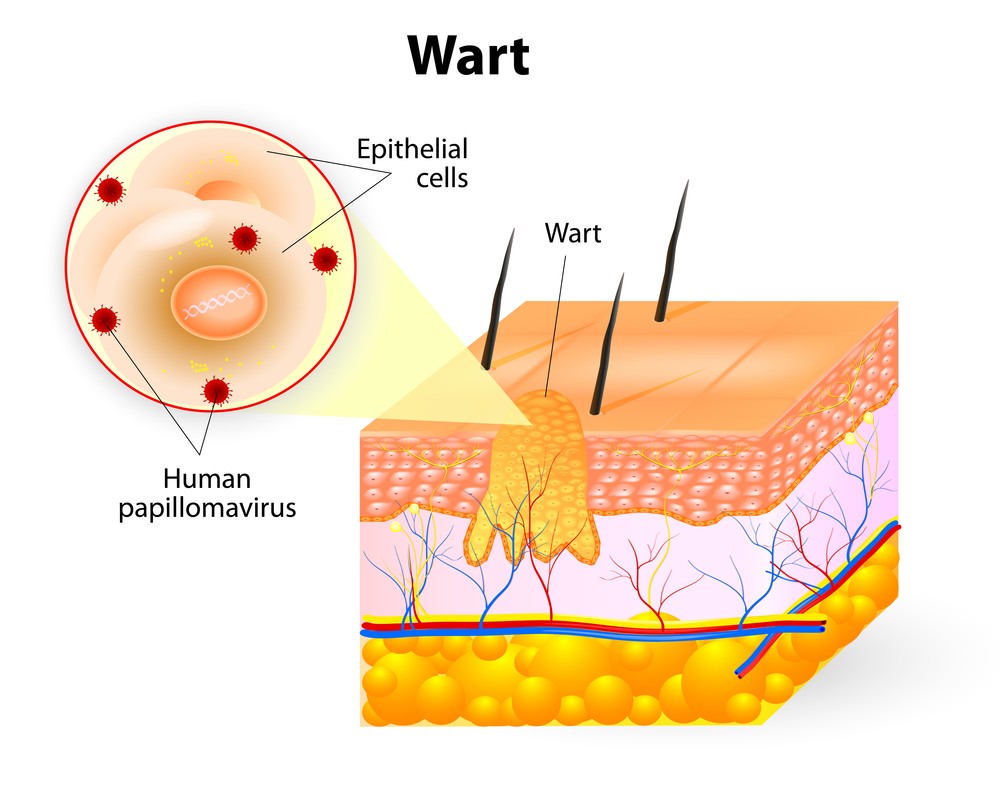
 Genital warts are one of the most common causes of sexually transmitted diseases (STDs) in the world. The human papillomavirus (HPV) is the virus that causes genital warts.
Genital warts are one of the most common causes of sexually transmitted diseases (STDs) in the world. The human papillomavirus (HPV) is the virus that causes genital warts.
HPV actually refers to a group of more than 60 viruses that have been identified by scientists and are responsible for warts anywhere on the body, but only certain types are sexually transmitted.
Experts estimate that as many as 26 million Americans are infected with HPV and the rate of infection appears to be increasing. About one-third of HPV-type viruses are spread through sexual contact and live only in genital areas of the body. Only one type of HPV causes genital warts. Other types of HPV cause cervical cancer and other genital cancers.
Like many sexually transmitted diseases, HPV usually causes a silent infection — one that does not have visible symptoms. People may not be aware of their infection or the potential risk of transmission to others and of the complications because they don’t know they have it.
Remember, genital warts are VERY CONTAGIOUS!
Symptoms
In women, the warts occur on the outside and inside of the vagina, labia, on the cervix (the opening to the uterus), around the anus or even on the thighs. In men, genital warts are less common. If present, they are seen on the tip of the penis sometimes they are also found on the shaft of the penis, on the scrotum, or around the anus. Rarely, genital warts also can develop in the mouth or throat of a person who has had oral sexual contact with an infected person.
The warts can appear as raised or flat, small or large, and single or clumped in a group that sometimes looks like cauliflower. Normally, the warts are flesh-colored or a bit lighter than your skin and painless. Less often they appear as slightly pink or gray. Rarely, they cause itching, pain, or bleeding.
Genital warts often occur in clusters and can be very tiny or can spread into large masses on genital tissues. Left untreated, genital warts often disappear. In other cases, they eventually may develop a fleshy, small raised growth with a cauliflower-like appearance. Because there is no way to predict whether the warts will grow or disappear, people who suspect that they have genital warts should be examined and treated.
Read Cervical Cancer article for more on the complications from HPV.
Incubation Period
About 2 to 4 months, but since infections are harder to get than bacterial ones, it can take from four to six weeks to infect a partner with HPV. In two-thirds of infected people, it can be up to nine months before any warts appear.
How Do You Know If You Have Them?
A health care provider usually can diagnose genital warts by direct visual examination. Women with genital warts also should be examined for possible HPV infection of the cervix. A Pap smear test also may indicate the possible presence of cervical HPV infection. A Pap smear is a microscopic examination of cells scraped from the uterine cervix in order to detect cervical cancer. (See our Pap Smear section for more info.) Abnormal Pap smear results are associated with HPV infection. Women with abnormal Pap smears should be examined further to detect and treat any cervical problems.
Treatment
 Depending on factors such as their size and location, genital warts are treated in several ways. Treatments can eliminate the warts, but none totally kill the virus and warts often reappear after treatment. You should consult your health care provider if you find genital warts on yourself or on your sexual partner(s).
Depending on factors such as their size and location, genital warts are treated in several ways. Treatments can eliminate the warts, but none totally kill the virus and warts often reappear after treatment. You should consult your health care provider if you find genital warts on yourself or on your sexual partner(s).
Treatments commonly include podophyllin solution, which is applied to the affected area and later wash off. Podophyllin (Pododerm, Podocon-25). that is applied by a doctor or a nurse, is best used on small, external warts. It is safe and relatively inexpensive, but causes some pain and discomfort at the area while it is on. It should not be used on large vulvar surfaces. Podophyllin needs to be washed off after one to four hours and you will need to be treated weekly for up to six weeks (in most cases). Very large amounts can cause harmful side effects, including nerve damage. Do not use this treatment if you are pregnant!
Small warts can be removed by cryosurgery (freezing), electrocautery (burning), or laser treatment. Occasionally, surgery is needed to remove large warts that have not responded to other treatment. Some health care providers use antiviral drugs which they inject directly into the warts, to treat warts that have recurred after removal by traditional means. The drug is expensive and does not reduce the rate of recurrence.
Letting the warts go away by themselves is actually an old treatment. Within three months, 20 to 30 percent of patients’ non-cervical warts will clear up by themselves. However, if you are sexually active this is not a good option for you as the virus is very contagious and even with a condom your vagina will have contact with your partner’s body, testicles, etc. So, get them treated!
I have seen warts get as big as a small cauliflower, I am serious. Those tend to be surgically removed, so get them treated.
Complications
Low-risk papilla viruses cause warts but not cervical cancer. High-risk viruses cause cervical cancer and also are associated with vulvar cancer, anal cancer, and cancer of the penis (a rare cancer). Although most HPV infections do not progress to cancer, it is particularly important for women who have cervical dysplasia to have regular Pap smears. Potentially precancerous cervical disease is readily treatable.
Prevention
The only way to prevent HPV infection is to avoid direct contact with the virus, which is transmitted by skin-to-skin contact. If warts are visible in the genital area, sexual contact should be avoided until the warts are treated. Using a latex condom during sexual intercourse may provide some protection and will usually prevent warts from being transmitted to the cervix, but that’s no guarantee.
Researchers are working to develop two types of HPV vaccines. One type would be used to prevent infection or disease (warts or precancerous tissue changes); another type would be used to treat cervical cancers. Clinical trials are in progress for both types of vaccines.
Update – July 2006: The vaccine Gardacil® protects agains four HPV types. These together cause 70% of cervical cancers and genital warts, according to the CDC. (Centers for Disease Control and Prevention).
This is good news, but does not mean you should stop using condoms to protect against STDs.
![]() Honest answers about orgasms, sexual health, stds and hundreds of sex faqs. Go There…
Honest answers about orgasms, sexual health, stds and hundreds of sex faqs. Go There…