Cervical Cancer — What is Cancer Anyway?
Cancer is a group of more than 100 different diseases. They all affect the body’s basic unit, the cell. Cancer occurs when cells become abnormal and divide without control.
 All of the organs of the body are made up of many types of cells. Normally, cells divide to produce more cells only when the body needs them. This orderly process helps keep us healthy. If cells keep dividing when new cells are not needed, a mass of tissue forms. This mass of extra tissue, called a growth or tumor, can be benign or malignant.
All of the organs of the body are made up of many types of cells. Normally, cells divide to produce more cells only when the body needs them. This orderly process helps keep us healthy. If cells keep dividing when new cells are not needed, a mass of tissue forms. This mass of extra tissue, called a growth or tumor, can be benign or malignant.
Benign tumors are not cancerous. They can usually be removed and, in most cases, they do not come back. The most important thing is that cells from benign tumors do not spread to other parts of the body. Benign tumors are not a threat to life. Polyps, cysts, and genital warts are types of benign growths of the cervix.
Malignant tumors are cancer. Cancer cells can invade and damage tissues and organs near the tumor. Cancer cells also can break away from a malignant tumor and enter the lymph system or the bloodstream. This is how cancer of the cervix can spread to other parts of the body, such as nearby lymph nodes, the rectum, the bladder, the bones of the spine, and the lungs. The spread of cancer is called metastasis.
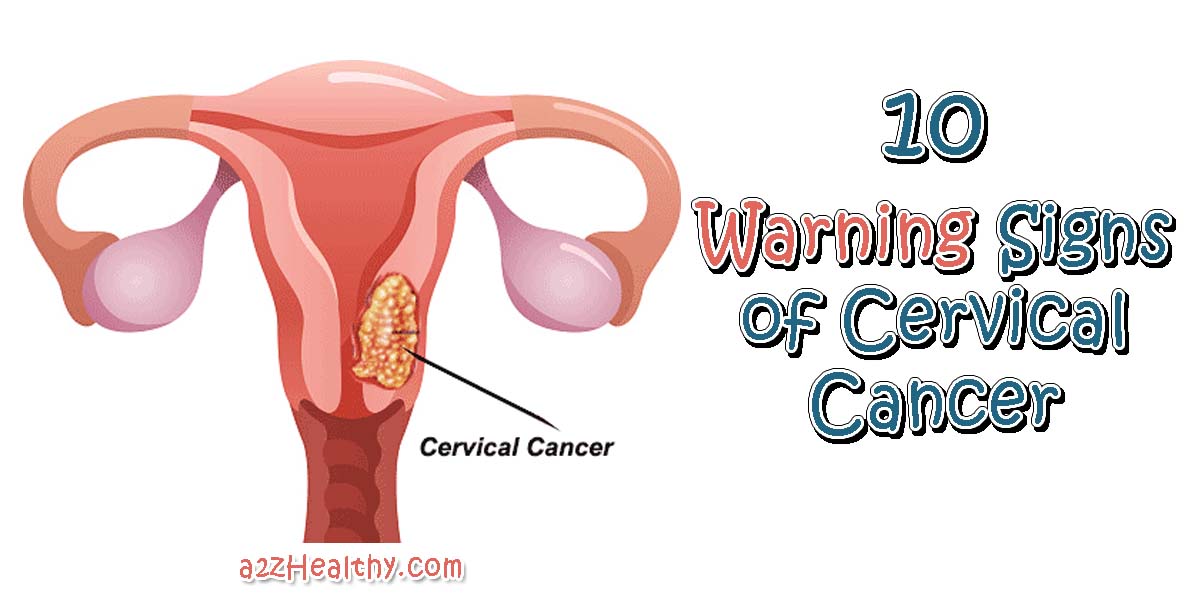
Like all other organs of the body, the cervix is made up of many types of cells. Normally, cells divide to produce more cells only when the body needs them. This orderly process helps keep us healthy. Cancer of the uterine cervix, the portion of the uterus that is attached to the top of the vagina. Ninety percent of cervical cancers arise from the flattened or “squamous” cells covering the cervix. Most of the remaining 10% arise from the glandular, mucus-secreting cells of the cervical canal leading into the uterus.
According to The National Cancer Institute, the vast majority of cervical cancers can be prevented. Since the most common form of cervical cancer starts with preventable and easily detectable precancerous changes, there are two ways to prevent this disease.
Here is a diagram showing where your cervix is located. The cervix is the lower, narrow part of the uterus. The cervix forms a canal that opens into the vagina, which leads to the outside of the body.
![]()
Causes and Risks
![]() Each year, about 15,000 women in the United States learn that they have cancer of the cervix.
Each year, about 15,000 women in the United States learn that they have cancer of the cervix.
The development of cervical cancer is gradual and begins as a pre-cancerous condition called dysplasia. In this form it is 100% treatable, usually without the need for hysterectomy.
Dysplasia, depending on its severity, can often resolve without treatment. More often it eventually progresses to actual cancer — called “carcinoma in situ” (CIS) when it has not yet spread, and “microinvasive” when it has spread only a few millimeters into the surrounding tissue and has not yet penetrated blood vessels and lymph channels.
This process may take many years, but once the cancer is established it quickly spreads further into the nearby tissues or to other organs, usually the intestines, liver, and lung. There are often no symptoms of cervical cancer until the disease is advanced.
The majority of women diagnosed today with cervical cancer have either not had regular Pap smears or they have not followed up after having an abnormal smear. Not having regular Pap smears is the single greatest risk factor for a bad outcome in women who develop cervical cancer.
Learn about Gardacil® – A Vaccine to Wipe out Cervical Cancer?
![]()
Risk factors for cervical cancer:
- Infection with human papilloma virus or HPV, the cause of genital warts. Not all women who have HPV infection develop cervical cancer. Scientists believe that certain other factors they call cofactors are involved in its development. One cofactor is smoking. Tobacco use damages the immune system and interferes with the body’s ability to resist HPV infection in the cervix.
- Multiple sexual partners and/or partners who have multiple partners.
- Early age of first sexual intercourse.
- In the early 1970’s, it was discovered that women whose mothers took an estrogen drug during pregnancy called DES (diethylstilbestrol) are at risk of a rare form of cervical and vaginal cancer. This drug was used from 1938 until 1971, and was sometimes combined with prenatal vitamins in the mistaken belief that it prevented miscarriages. If you are old enough to be a “DES baby”, ask your mother if she ever was given this drug. For more information go to the DES Action web page.
- There is a small increased risk of abnormal Pap smears among women who take birth control pills. It is thought that this is because such women are more sexually active, are less likely to use condoms, and have more frequent Pap smears in order to be prescribed the birth control pill.
- Women whose immune systems are weakened, such as those with HIV infection or women who have received organ transplants and are taking drugs to suppress the immune system may be at a higher risk.
- Infections with genital herpes or chronic Chlamydia infections, both STDs, may increase risk
- Poor women may be at higher risk because they are not able to afford regular pap smears. Worldwide, cervical cancer is the third most common type of cancer in women. It is much less common in the US, where it has been declining. This is due almost entirely to the use of the Pap smear, which has reduced the death rate from this disease by 70% since it was introduced in 1941. Yet according to the American Cancer Society, 12,800 women were diagnosed with cervical cancer in the year 2000, and there were 4,600 deaths from this disease.
![]()
Symptoms
Precancerous changes of the cervix usually do not cause pain. In fact, they generally do not cause any symptoms and are not detected unless a woman has a pelvic exam and a Pap test.
Symptoms usually do not appear until abnormal cervical cells become cancerous and invade nearby tissue. When this happens, the most common symptom is abnormal bleeding. Bleeding may start and stop between regular menstrual periods, or it may occur after sexual intercourse, douching, or a pelvic exam. Menstrual bleeding may last longer and be heavier than usual. Bleeding after menopause also may be a symptom of cervical cancer. Increased vaginal discharge is another symptom of cervical cancer.
These symptoms may be caused by cancer or by other health problems. Only a doctor can tell for sure. It is important for a woman to see her doctor if she is having any of these symptoms.
![]()
Can Cervical Cancer Be Prevented?
Many cases can be prevented! The vast majority of cervical cancers can be prevented. Since the most common form of cervical cancer starts with preventable and easily detectable precancerous changes, there are two ways to prevent this disease.
Cervical Cancer – Can It Be Prevented?
Yes. According to The National Cancer Institute, the vast majority of cervical cancers can be prevented. Since the most common form of cervical cancer starts with preventable and easily detectable precancerous changes, there are two ways to prevent this disease.
The first way is to prevent precancers. Most precancers of the cervix can be prevented by avoiding risk factors. Delaying the onset of sexual intercourse if you are young can help avoid HPV infection. In addition, limiting your number of sexual partners and avoiding sex with people who have had a lot of sexual partners decreases your risk of exposure to HPV.
 HPV infection does not always produce warts or other symptoms, so a person may be infected with HPV and pass it on without knowing. Recent research shows that condoms cannot protect against infection with HPV. Why? Because HPV can be passed from person to person with any skin to skin contact with any HPV infected area of the body, such as skin of the genital or anal area not covered by the condom.
HPV infection does not always produce warts or other symptoms, so a person may be infected with HPV and pass it on without knowing. Recent research shows that condoms cannot protect against infection with HPV. Why? Because HPV can be passed from person to person with any skin to skin contact with any HPV infected area of the body, such as skin of the genital or anal area not covered by the condom.
The absence of visible warts cannot be used to decide whether caution is warranted, since HPV can be passed on to another person even when there are no visible warts or other symptoms. HPV can be present for years with no symptoms. It is still important, though, to use condoms to protect against AIDS and other sexually transmitted diseases that are passed on through some body fluids. Not smoking is another way to reduce the risk of cervical cancer and precancer.
The second way to prevent invasive cancer is to have a Pap test to detect HPV infection and precancers. Treatment of these disorders can stop cervical cancer before it is fully developed. Most invasive cervical cancers are found in women who have not had regular Pap tests.
The American Cancer Society recommends that all women begin yearly Pap tests at age 18 or when they become sexually active, whichever occurs first. If a woman has had three negative annual Pap tests in a row, this test may be done less often at the judgment of a woman’s health care provider.
If a hysterectomy was done for cancer, more frequent Pap tests may be recommended. Some women believe they do not have to be examined by a health care provider once they have stopped having children. This is not correct. They should continue to follow ACS guidelines.
It is important to remember that while the Pap test has been more successful than any other screening test in preventing a cancer, it is not perfect. Because some abnormalities may be missed (even when samples are examined in the best laboratories), it is not a good idea to have this test less often than ACS guidelines recommend.
![]()
How a Pap Test Is Done
The health care provider first inserts a speculum, a metal or plastic instrument that keeps the vagina open so that the cervix can be seen clearly. Next, a sample of cells and mucus is lightly scraped from the ectocervix using a small spatula. A small brush or a cotton tipped swab is used to take a sample from the endocervix. These samples are then smeared on glass slides. The slides are sent to the lab where specially trained technologists and doctors examine the samples under a microscope. For more on pap tests see our papsmear page.
![]()
Additional Tests for Women with Abnormal Pap Test Results
Because the Pap test is a screening test rather than a diagnostic test, patients with abnormal Pap test results have additional tests (colposcopy and biopsy) to find out whether a precancerous change or cancer is present. If the biopsy shows SIL or dysplasia, steps will be taken to prevent progression to an actual cancer.
Colposcopy
If certain symptoms suggest cancer or if the Pap test shows abnormal cells, your health care provider may perform an additional test called a colposcopy. In this procedure the cervix is viewed through a colposcope, an instrument with magnifying lenses very much like binoculars. The colposcope makes it possible to see the surface of the cervix closely and clearly. The exam is not painful, has no side effects, and it can be performed safely throughout pregnancy. If abnormal areas are seen on the cervix, a biopsy (removal of a small tissue sample) is done. This is examined under the microscope by a pathologist.. If an abnormal area is seen by colposcopy, a biopsy is the only way to tell for certain whether you have a precancer, a true cancer, or neither.
Cervical Biopsies
There are several types of biopsies used to diagnose cervical precancers and cancers. For precancers and early cancers, some types of biopsies can completely remove the abnormal tissue and may be the only treatment needed. In some situations, additional treatment of precancers or cancers is needed.
Colposcopic biopsy: For this type of biopsy, a doctor or other health care provider first examines the cervix with a colposcope. This instrument uses magnifying binoculars to help find abnormal areas. A biopsy forceps is used to remove a small (about 1/8 inch) section of the abnormal area on the surface of the cervix. The biopsy procedure may cause mild cramping or brief pain, and there may be light bleeding afterwards. A local anesthetic may be used to numb the cervix.
Endocervical curettage (endocervical scraping): This procedure is usually done during the same session as the colposcopic biopsy. A narrow instrument (the curette) is inserted into the endocervical canal (the passage between the outer part of the cervix and the inner part of the uterus). Some of the tissue lining the endocervical canal is removed by scraping with the curette and sent to the laboratory. Because the colposcope views only the outer part of the cervix and cannot see into the endocervix , health care providers use the endocervical scraping to find out if this area is affected by precancer or cancer. A local anesthetic may be used to numb the cervix. Patients may have a temporary cramping sensation, similar to a severe menstrual cramp. There may be light bleeding after the procedure.
Cone biopsy: This procedure removes a cone-shaped piece of tissue from the cervix. The base of the cone is formed by the ectocervix (outer part of the cervix), and the point or apex of the cone is from the endocervical canal. The transformation zone (the border between the ectocervix and endocervix) is contained within the cone. This is the area of the cervix where precancers and cancers are most likely to develop. The cone biopsy is also a treatment, and can completely remove many precancers and very early cancers. There are two methods commonly used for cone biopsies, the loop electrosurgical excision procedure (LEEP or LLETZ) and the cold knife cone biopsy.
The LEEP (LLETZ) removes tissue with a wire that is heated by electrical current. This procedure uses a local anesthetic, and can be done in your doctor’s office. It takes only about 10 minutes. There may be mild cramping during and after the procedure, and mild to moderate bleeding may persist for several weeks. The cold knife cone biopsy uses a surgical scalpel or a laser as a scalpel, rather than a heated wire to remove tissue. It requires general anesthesia (you are asleep during the operation). It is done in a hospital, but no overnight stay is needed. After the procedure, cramping and some bleeding may persist for a few weeks.
![]()
How Patients with Abnormal Pap Results Are Treated to Prevent Cancers from Developing
 If an area of SIL can be seen during the colposcopy, your doctor will be able to remove the abnormal area by using such biopsy techniques as the LEEP (LLETZ) technique or a cold knife cone biopsy or by destroying the abnormal cells with cryosurgery or laser surgery. During cryosurgery a metal probe cooled with liquid nitrogen is used to kill the abnormal cells by freezing them. Laser surgery uses a focused beam of high energy light to vaporize the abnormal tissue. Both of these are outpatient treatments that can be done in a doctor’s office or clinic. After treatment, women may have a watery brown discharge for a few weeks.
If an area of SIL can be seen during the colposcopy, your doctor will be able to remove the abnormal area by using such biopsy techniques as the LEEP (LLETZ) technique or a cold knife cone biopsy or by destroying the abnormal cells with cryosurgery or laser surgery. During cryosurgery a metal probe cooled with liquid nitrogen is used to kill the abnormal cells by freezing them. Laser surgery uses a focused beam of high energy light to vaporize the abnormal tissue. Both of these are outpatient treatments that can be done in a doctor’s office or clinic. After treatment, women may have a watery brown discharge for a few weeks.
These treatments are almost always effective in destroying precancers and preventing them from developing into true cancers. Follow-up examinations will be needed to make sure that the abnormality does not come back. If it does, treatments can be repeated. If you have had abnormal pap resutls, discuss this with your health care provider and a gynecologist and together decide what approach you would like to take.
Thanks are extending to the The National Cancer Institute for the information provided on this topic. Visit them at cancer.gov