Bipolar Disorder
 Bipolar disorder, also known as manic-depressive illness, is a brain disorder that causes unusual shifts in a person’s mood, energy, and ability to function. Different from the normal ups and downs that everyone goes through, the symptoms of bipolar disorder are severe and can result in damaged relationships, poor job or school performance, and even suicide. There is good news: bipolar disorder can be treated, and people with this illness can lead full and productive lives.
Bipolar disorder, also known as manic-depressive illness, is a brain disorder that causes unusual shifts in a person’s mood, energy, and ability to function. Different from the normal ups and downs that everyone goes through, the symptoms of bipolar disorder are severe and can result in damaged relationships, poor job or school performance, and even suicide. There is good news: bipolar disorder can be treated, and people with this illness can lead full and productive lives.
More than two million American adults, or about one percent of the population age 18 and older in any given year have bipolar disorder. Bipolar disorder typically develops in late adolescence or early adulthood. However, some people have their first symptoms during childhood, and some develop them late in life. It is often not recognized as an illness, and people may suffer for years before it is properly diagnosed and treated. Like diabetes or heart disease, bipolar disorder is a long-term illness that must be carefully managed throughout a person’s life.
“Manic-depression distorts moods and thoughts, incites dreadful behaviors, destroys the basis of rational thought, and too often erodes the desire and will to live. It is an illness that is biological in its origins, yet one that feels psychological in the experience of it; an illness that is unique in conferring advantage and pleasure, yet one that brings in its wake almost unendurable suffering and, not infrequently, suicide.
“I am fortunate that I have not died from my illness, fortunate in having received the best medical care available, and fortunate in having the friends, colleagues, and family that I do.”
Kay Redfield Jamison, Ph.D., An Unquiet Mind, 1995, p. 6. (Reprinted with permission from Alfred Knopf, – division of Random House, Inc.)
What Are the Symptoms of Bipolar Disorder?
Bipolar disorder causes dramatic mood swings from overly “high” and/or irritable to sad and hopeless, and then back again, often with periods of normal mood in between. Severe changes in energy and behavior go along with these changes in mood. The periods of highs and lows are called episodes of mania and depression.
Signs and Symptoms of Mania (or manic episode) include:
- Increased energy, activity, and restlessness
- Excessively “high”, overly good, euphoric mood
- Extreme irritability
- Racing thoughts and talking very fast, jumping from one idea
- to another
- Distractibility, unable to concentrate well
- Little sleep needed
- Unrealistic beliefs in ones abilities and powers
- Poor judgment
- Spending sprees
- A lasting period of behavior that is different from usual
- Increased sexual drive
- Abuse of drugs, particularly cocaine, alcohol, and sleeping
medications - Provocative, intrusive, or aggressive behavior
- Denial that anything is wrong
A manic episode is diagnosed if elevated mood occurs with three or more of the other symptoms most of the day, nearly every day, occurring one week or longer. If the mood is irritable, four additional symptoms must be present.
![]()
Signs and symptoms of depression (or a depressive episode) include:
- Lasting sad, anxious, or empty mood
- Feelings of hopelessness or pessimism
- Feelings of guilt, worthlessness, or helplessness
- Loss of interest or pleasure in activities once enjoyed,
including sex - Decreased energy, a feeling of fatigue or of being slowed
down - Difficulty concentrating, remembering, making decisions
- Restlessness or irritability
- Sleeping too much, or insomnia
- Change in appetite and/or unintended weight loss or gain
- Chronic pain or other persistent bodily symptoms that are not
caused by physical illness or injury - Thoughts of death or suicide, or suicide attempts
- A depressive episode is diagnosed if 5 or more of these symptoms last most of the day, nearly every day, for a period of two weeks or longer.
A mild to moderate level of mania is called hypomania. Hypomania may feel good to the person who experiences it and may even be associated with good functioning and enhanced productivity. Thus even when family and friends learn to recognize the mood swings as possible bipolar disorder, the person may deny that anything is wrong. Without proper treatment, however, hypomania can become severe mania in some people or can switch into depression.
Sometimes, severe episodes of mania or depression include symptoms of psychosis (or psychotic symptoms). Common psychotic symptoms are hallucinations (hearing, seeing, or otherwise sensing the presence of things not actually there) and delusions (false, strongly held beliefs not influenced by logical reasoning or explained by a person’s usual cultural concepts). Psychotic symptoms in bipolar disorder tend to reflect the extreme mood state at the time. For example, delusions of grandiosity, such as believing one is the President or has special powers or wealth, may occur during mania; delusions of guilt or worthlessness, such as believing that one is ruined and penniless or has committed some terrible crime, may appear during depression. People with bipolar disorder who have these symptoms are sometimes incorrectly diagnosed as having schizophrenia.
It may be helpful to think of the various mood states in bipolar disorder as a spectrum or continuous range. At one end is severe depression, then there is normal or balanced mood, above which comes hypomania (mild to moderate mania), and then severe mania.
In some people, however, symptoms of mania and depression may occur together in what is called a mixed bipolar state. Symptoms of a mixed state often include agitation, trouble sleeping, significant change in appetite, psychosis, and suicidal thinking. A person may have a very sad, hopeless mood while at the same time feeling extremely energized.
Bipolar disorder may appear to be a problem other than mental illnes, for instance, alcohol or drug abuse, poor school or work performance, or strained interpersonal relationships. These problems in fact may be signs of an underlying mood disorder.
![]()
Diagnosis of Bipolar Disorder
Like other mental illnesses, bipolar disorder cannot yet be identified physiologically, for example, through a blood test or a brain scan. Therefore, a diagnosis of bipolar disorder is made on the basis of symptoms, course of illness, and, when available, family history. The diagnostic criteria for bipolar disorder are described in the Diagnostic and Statistical Manual for Mental Disorders, fourth edition (DSM-IV). Descriptions offered by people with bipolar disorder give valuable insights into the various mood states associated with the illness:
Depression: I doubt completely my ability to do anything well. It seems as though my mind has slowed down and burned out to the point of being virtually useless”. [I am] haunt[ed]”with the total, the desperate hopelessness of it all”. Others say, “It’s only temporary, it will pass, you will get over it,” but of course they haven’t any idea of how I feel, although they are certain they do. If I can’t feel, move, think or care, then what on earth is the point?
Hypomania: “At first when I’m high, it’s tremendous… ideas are fast… like shooting stars you follow until brighter ones appear. All shyness disappears, the right words and gestures are suddenly there… uninteresting people, things become intensely interesting. Sensuality is pervasive, the desire to seduce and be seduced is irresistible. Your marrow is infused with unbelievable feelings of ease, power, well-being, omnipotence, euphoria… you can do anything… but, somewhere this changes”.
Mania: The fast ideas become too fast and there are far too many. Overwhelming confusion replaces clarity… you stop keeping up with it. Your memory goes. Your friends become frightened…everything is now against the grain, you are irritable, angry, frightened, uncontrollable, and trapped”.
Suicide Risk
Some people with bipolar disorder become suicidal. Anyone who is thinking about committing suicide needs immediate attention, preferably from a mental health professional or a physician, or a school counselor. Risk for suicide appears to be higher earlier in the course of the illness. Therefore, recognizing bipolar disorder early and learning how best to manage it may decrease the risk of death by suicide.
Anyone who talks about suicide should be taken seriously. See suicide for hotlines to call for immediate help.
Signs and symptoms that may accompany suicidal feelings include:
- Talking about feeling suicidal or wanting to die
- Feeling hopeless, that nothing will ever change or get better
- Feeling helpless
- Feeling like a burden to family and friends
- Abusing alcohol or drugs
- Putting affairs in order (e.g. giving away possessions, or organizing finances to prepare for one’s death)
- Writing a suicide note
- Putting oneself in harm’s way
If you are feeling suicidal or know someone who is:
- Call a doctor, emergency room, or 911 right away to get immediate help
- Make sure you, or the suicidal person, are not left alone
- Make sure that access is prevented to large amounts of medication, weapons, or other items that could be used for self-harm
While some suicide attempts are carefully planned over time, others are impulsive acts that have not been well thought out; thus, the final point in the box above may be a valuable long-term strategy for people with bipolar disorder. Either way, it is important to understand that suicidal feelings and actions are symptoms of an illness that can be treated. With proper treatment, suicidal feelings can be overcome.
What is the Course of Bipolar Disorder?
Episodes of mania and depression typically recur across the life span. Between episodes, most people with bipolar disorder are free of symptoms, but as many as one-third of people have some residual symptoms. A small percentage of people experience chronic unremitting symptoms despite treatment.
The classic form of the illness, which involves recurrent episodes of mania and depression, is called bipolar I disorder. Some people, however, never develop severe mania but instead experience milder episodes of hypomania that alternate with depression; this form of the illness is called bipolar II disorder. When four or more episodes of illness occur within a 12-month period, a person is said to have rapid-cycling bipolar disorder. Some people experience multiple episodes within a single week, or even within a single day. Rapid cycling tends to develop later in the course of illness and is more common among women than among men.
People with bipolar disorder can lead healthy and productive lives when the illness is effectively treated. Without treatment, however, the natural course of bipolar disorder tends to worsen. Over time a person may suffer more frequent (more rapid-cycling) and more severe manic and depressive episodes than those experienced when the illness first appeared. But in most cases, proper treatment can help reduce the frequency and severity of episodes and can help people with bipolar disorder maintain good quality of life.
Can Children and Adolescents Have Bipolar Disorder?
Yes. Both children and adolescents can develop bipolar disorder. It is more likely to affect the children of parents who have the illness. Unlike many adults with bipolar disorder, whose episodes tend to be more clearly defined, children and young adolescents with the illness often experience very fast mood swings between depression and mania many times within a day. Children with mania are more likely to be irritable and prone to destructive tantrums than to be overly happy and elated. Mixed symptoms also are common in youths with bipolar disorder. Older adolescents who develop the illness may have more classic, adult-type episodes and symptoms.
Bipolar disorder in children and adolescents can be hard to tell apart from other problems that may occur in these age groups. For example, while irritability and aggressiveness can indicate bipolar disorder, they also can be symptoms of attention deficit hyperactivity disorder, conduct disorder, oppositional defiant disorder, or other types of mental disorders more common among adults such as major depression or schizophrenia.
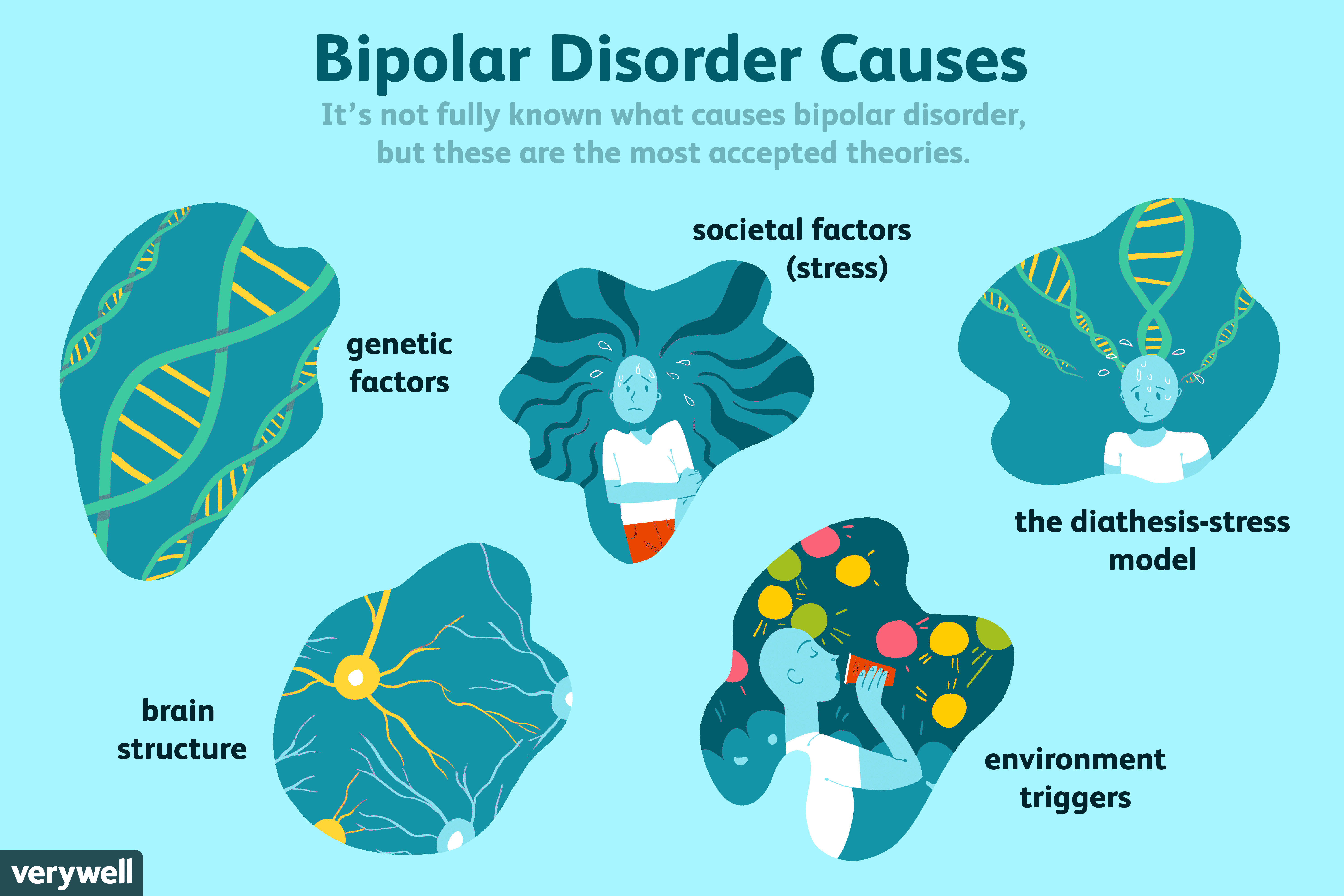
What Causes Bipolar Disorder?
Scientists are learning about the possible causes of bipolar disorder through several kinds of studies. Most scientists now agree that there is no single cause for bipolar disorder. Many factors act together to produce the illness.
Because bipolar disorder tends to run in families, researchers have been searching for specific genes that may increase a person’s chance of developing the illness. But genetics are not the whole story. Studies of identical twins, who share all the same genes, indicate that both genes and other factors play a role in bipolar disorder. If bipolar disorder were caused entirely by genes, then the identical twin of someone with the illness would always develop the illness, and research has shown that this is not the case. But if one twin has bipolar disorder, the other twin is more likely to develop the illness than is another sibling.
In addition, findings from gene research suggest that bipolar disorder, like other mental illnesses, does not occur because of a single gene. It appears likely that many different genes act together, and in combination with other factors of the person or the person’s environment to cause bipolar disorder.
Brain-imaging studies are helping scientists learn what goes wrong in the brain to produce bipolar disorder and other mental illnesses. There is evidence from imaging studies that the brains of people with bipolar disorder may differ from the brains of healthy individuals. As the differences are more clearly identified and defined through research, scientists will gain a better understanding of the underlying causes of the illness, and eventually may be able to predict which types of treatment will work most effectively.
![]()
How is Bipolar Disorder Treated?
Most people with bipolar disorder even those with the most severe forms can achieve substantial stabilization of their mood swings and related symptoms with proper treatment. Because bipolar disorder is a recurrent illness, long-term preventive treatment is strongly recommended and almost always indicated. A strategy that combines medication and psychosocial treatment is optimal for managing the disorder over time.
In most cases, bipolar disorder is much better controlled if treatment is continuous than if it is on and off. But even when there are no breaks in treatment, mood changes can occur and should be reported immediately to your doctor. The doctor may be able to prevent a full-blown episode by making adjustments to the treatment plan.
Working closely with the doctor and communicating openly about treatment concerns and options can make a difference in treatment effectiveness. In addition, keeping a chart of daily mood symptoms, treatments, sleep patterns, and life events may help people with bipolar disorder and their families to better understand the illness. This chart also can help the doctor track and treat the illness most
effectively.
![]()
Medications
Medications for bipolar disorder are prescribed by psychiatrists, medical doctors and nurse practitioners with expertise in the diagnosis and treatment of mental disorders. While primary care physicians who do not specialize in psychiatry also may prescribe these medications, it is recommended that people with bipolar disorder see a psychiatrist for treatment.
Medications known as ‘mood stabilizers’ usually are prescribed to help control bipolar disorder. Several different types of mood stabilizers are available. In general, people with bipolar disorder continue treatment with mood stabilizers for extended periods of time (years). Other medications are added when necessary, typically for shorter periods, to treat episodes of mania or depression that break through despite the mood stabilizer. Lithium, the first mood-stabilizing medication approved by the U.S. Food and Drug Administration (FDA) for treatment of mania, is often very effective in controlling mania and preventing the recurrence of both manic and depressive episodes.
Anticonvulsant medications, such as valproate (Depakote) or carbamazepine (Tegretol), also can have mood-stabilizing effects and may be especially useful for difficult-to-treat bipolar episodes.
Newer anticonvulsant medications, including lamotrigine (Lamictal), gabapentin (Neurontin), and topiramate (Topamax), are being studied to determine how well they work in stabilizing mood cycles. Aripiprazole (Abilify) is indicated for the treatment of schizophrenia and acute manic and mixed episodes associated with bipolar disorder.
Atypical antipsychotic medications, including clozapine (Clozaril), olanzapine (Zyprexa), risperidone (Risperdal), and ziprasidone (Zeldox), are being studied as possible treatments for bipolar disorder. Evidence suggests clozapine may be helpful as a mood stabilizer for people who do not respond to lithium or anticonvulsants. Other research has supported the efficacy of other drugs for acute mania.
Medication Side Effects
Before starting a new medication for bipolar disorder, always talk with your psychiatrist and/or pharmacist about possible side effects. Depending on the medication, side effects may include weight gain, nausea, tremor, reduced sexual drive or performance, anxiety, hair loss, movement problems, or dry mouth. Be sure to tell the doctor about all side effects you notice during treatment. He or she may be able to change the dose or offer a different medication to relieve them. Your medication should not be changed or stopped without the psychiatrist’s guidance.
Psychosocial Treatments
As an addition to medication, psychosocial treatment including certain forms of psychotherapy are helpful in providing support, education, and guidance to people with bipolar disorder and their families. Studies have shown that psychosocial interventions can lead to increased mood stability, fewer hospitalizations, and improved functioning in several areas. A licensed psychologist, social worker, or counselor typically provides these therapies and often works together with the psychiatrist to monitor a patient’s progress. The number, frequency, and type of sessions should be based on the treatment needs of each person.
Psychosocial interventions commonly used for bipolar disorder are cognitive behavioral therapy, psychoeducation, family therapy, and a newer technique, interpersonal and social rhythm therapy. NIMH researchers are studying how these interventions compare to one another when added to medication treatment for bipolar disorder. Cognitive behavioral therapy helps people with bipolar disorder learn to change inappropriate or negative thought patterns and behaviors associated with the illness.
Psychoeducation involves teaching people with bipolar disorder about the illness and its treatment, and how to recognize signs of relapse so that early intervention can be sought before a full-blown illness episode occurs. Psycho-education also may be helpful for family members. Family therapy uses strategies to reduce the level of distress within the family that may either contribute to or result from the ill person’s symptoms.
As with medication, it is important to follow the treatment plan for any psychosocial intervention to achieve the greatest benefit.
![]()
Resources for More Information
National Institute of Mental Health (NIMH)
8184, MSC 9663
Bethesda, MD 20892-9663
Phone: (301) 443-4513
Web site: http://www.nimh.nih.gov
Child & Adolescent Bipolar Foundation
1187 Wilmette Avenue
Wilmette, IL 60091
Phone: (847) 256-8525
Web site: http://www.bpkids.org
Depression and Related Affective Disorders Association (DRADA)
Johns Hopkins Hospital,
Meyer 3-181
600 North Wolfe Street
Baltimore, MD 21287-7381
Web site: http://www.drada.org
National Alliance for the Mentally Ill (NAMI)
Colonial Place Three
2107 Wilson Blvd., 3rd
Arlington, VA 22201-3042
Toll-Free: 1-800-950-NAMI (6264)
Phone: (703) 524-7600; Fax: (703) 524-9094
Web site: http://www.nami.org
Depression & Bipolar Support Alliance (DBSA)
730 North Franklin Street
Chicago, IL 60610-7204
Toll-Free: 1-800-826-3632
Phone: (312) 642-0049; Fax: (312) 642-7243
Web site: http://www.DBSAAlliance.org
National Foundation for Depressive Illness, Inc. (NAFDI)
P.O. Box 2257
New York, NY 10116
Toll-Free: 1-800-239-1265
Web site: http://www.depression.org
National Mental Health Association (NMHA)
2001 N Beauregard Street
12th floor Alexandria, VA 22311
1-800-969-NMHA (6642)
Phone: (703) 684-7722;
Fax: (703) 684-5968
Web site: http://www.nmha.org
[Source: National Institute of Mental Health]